How Does Applied Economics Maximize Kidney Transplants?
A project aimed at expanding kidney exchange and saving lives puts Nobel Prize-winning matching theory into practice

In the year 2000, there were 13,600 kidney transplants in the United States. Just 22 years later, that number topped 25,000—in part because of some creative thinking from Dr. Alvin E. Roth, an economist and Stanford University professor in the School of Humanities and Sciences, and his colleagues.
There are currently more than 96,000 people waiting for a kidney in the U.S., according to data from United Network for Organ Sharing (UNOS), a non-profit organization that manages the national organ transplant list for the U.S. federal government. Despite more transplants being performed year over year, a person is added to the transplant list every 10 minutes, which means demand currently outpaces supply.
For decades after the first successful kidney transplants in 1954, there were essentially two ways to get a new kidney: match with a deceased organ donor, or find a living donor who matched with you—typically a family member or friend.
In short, your options were limited until Roth applied his understanding of matching markets to the problem of how to get more kidneys to more patients, work for which, in part, he won the Nobel Prize in Economic Sciences.
New Models, More Options
Roth and colleagues realized there was lost potential in the family member or friend who is willing to donate a kidney, yet isn’t a match for the person in need. The researchers pioneered work on paired kidney exchange in New England in the early 2000s, introducing algorithmic models that matched incompatible donor/candidate pairs with the candidate of another pair and vice versa. (For example, if I need a kidney and my sister is willing to give me one but isn’t a match, we could be paired with someone who my sister matched with if their living donor matched with me.)
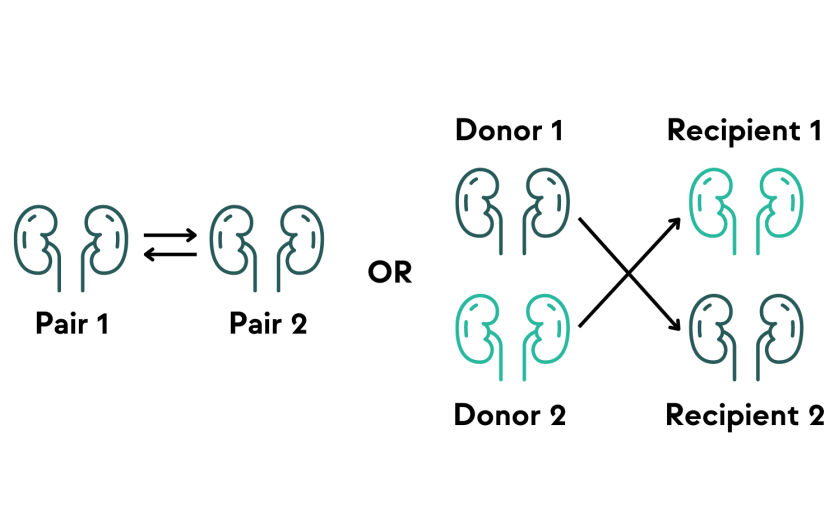
This model increased the number of kidney transplants, but the practice was difficult to scale because all the operations had to take place nearly simultaneously to ensure everyone involved got the kidney they were promised. (I don’t want to let you have my sister’s kidney unless I’m sure your son is going to give me his.) This limited the number of exchanges to 3 or 4 pairs maximum.
In 2006, paired kidney donation expanded into a “domino chain,” which introduced a non-directed or altruistic donor (an individual willing to give a kidney to a stranger) into the equation, increasing the pool of kidneys available. But because the operations were still done on the same day to avoid the chance of the chain being broken and someone losing out on getting a kidney, it was still impossible to scale.
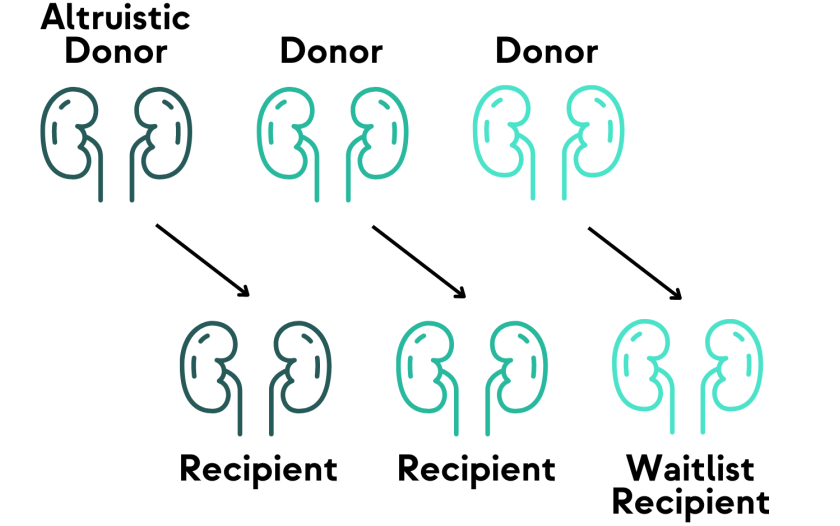
In 2007, Roth and colleagues, among them Dr. Michael Rees, transplant surgeon and founder of the Alliance for Paired Kidney Donation (APKD), expanded on the domino chain model by introducing non-simultaneous, extended, altruistic donor (NEAD) chains. The model resembles the domino chain, but drops the requirement that all the operations need to take place simultaneously. Instead, it trusts that people will fulfill their promise to donate a kidney at a future date to keep the chain going, which allows for gaps of time between surgeries.
Since each pair in a NEAD chain receives a kidney before they give one, there is some security baked into the model. If, for some reason, the chain breaks, a pair is able to participate in a chain at a later time because they still have a kidney to give.
The model has proven successful. APKD uses open source software developed by Itai Ashlagi, Professor of Management Science and Engineering at Stanford University, to facilitate the matching process for its NEAD chains, and they currently average 5 non-simultaneous transplants per chain. The longest chain recorded in the U.S. resulted in 35 transplants.
Roth and APKD are recipients of a Stage 3 investment from Stanford Impact Labs, which provides funding to put specific insights to use across multiple contexts at scale. In this case, Roth, APKD, and a team of partners coalesced to form Extending Kidney Exchange, a project designed to expand this work on two fronts: by (1) partnering with Walter Reed National Military Medical Center to use deceased donors to start NEAD chains, and (2) helping to expand access to kidney exchange in India and Brazil.
Expanding Chains in the U.S. With Deceased Donors
According to Roth, rules around using deceased donor kidneys are quite strict—those kidneys are not currently available to initiate a NEAD chain. “We are lucky to be able to partner with Walter Reed because they have a slightly different set of rules around deceased donor kidneys. They operate under what is called a military share, and recently modified rules mean they can work with us to study how introducing deceased donors into NEAD chains can increase kidney exchange in the U.S.”
“Walter Reed has been participating in NEAD chains with living altruistic donors since 2016,” said Rees. “This investment from SIL will allow APKD to continue our work with Walter Reed and the organ procurement organization Life Connection of Ohio so we have proof of principle that utilizing a deceased donor kidney to initiate a chain will result in a higher number of transplants, in this case for both civilians and military personnel. We hope to eventually influence policy so other organ procurement organizations can participate too.”
Dr. Jamie Diaz Robinson, Lieutenant Colonel in the Army and the Chief of Organ Transplant Services at Walter Reed, sees this project as an opportunity to expand access to organs for their patients as well as those outside their network. “As a small entity, and the only transplant center in the Department of Defense, we don’t have a large internal network from which patients can access organs,” she said. “This collaboration will expand access to organs and reduce wait times for our patients, and we hope it will also show people that donating just one kidney can start a chain that will have a ripple effect that saves many lives.”
Supporting Kidney Exchange in India and Brazil
Additionally, the SIL Stage 3 award will allow the team to respond to demand for paired kidney exchange in India and Brazil, two countries with extremely restrictive rules around organ donation designed to prevent black market organ trafficking.
“Making transplants available legally, safely, and ethically is the best way to compete with black markets in both countries,” said Roth, who points to the example of the collapse of black market alcohol production upon the end of prohibition in the U.S. in the 1930s.
“In both locations, we’re using everything we’ve learned from 25 years of doing this work in the United States to hopefully jumpstart similar programs in these countries,” said Rees. “There is tremendous opportunity if we can get kidney exchange to work in both these places, and SIL funding will help us figure out how to do it legally and ethically, and help our international colleagues build policies to support it.”
India has limited deceased donor programs, and current policies prioritize living donations from relatives. If you wish to receive a kidney from a friend or stranger, you have to seek permission from an authorization committee, a process which can be inconsistent from one region to the next, according to Rees.
“India has the third highest number of kidney transplants in the world (after the U.S. and China), and they have also been successfully experimenting with paired exchanges. Because its population is so large, there is real potential to save a lot of lives by introducing chains there,” Roth explained.
APKD’s partner in India is Vivek Kute, a professor of nephrology and transplantation at the Institute of Kidney Diseases and Research Center and Dr. H L Trivedi Institute of Transplantation Sciences (IKDRC-ITS) in Ahmedabad. Professor Kute hopes to double the number of transplants at IKDRC-ITS in 2024. “The expertise, software, and human resources available to us from APKD are critical to helping us offer better services, education, and research,” said Professor Kute. “We hope the results of this collaboration set us up for sustained growth and start to shift the perception of policy makers.”
Like India, Brazil performs a large number of kidney transplants, but laws restrict patients to transplants from deceased donors, living relatives, or spouses. Brazilian law does not allow paired exchanges initiated by altruistic donors.
“Our collaborators in Brazil have permission to do a clinical trial for paired exchanges under supervision—each exchange will have to be approved by a judge. We expect it to be quite successful,” said Roth.
Dr. Gustavo Fernandes Ferreira, President of the Brazilian Association of Organ Transplantation (ABTO) and the Medical Director of Pancreas and Kidney Transplant Program at Santa Casa de Misericórdia Juiz de Fora, describes a number of unique challenges to increasing kidney transplants. “There are ethical and legal challenges, infrastructure and resource issues, cultural and religious barriers, and financial constraints in Brazil, but, if each is addressed effectively, we can improve the availability and success of transplants for more people,” Ferreira said.
“We are in the process of setting specific goals right now, but, generally speaking, establishing a sustainable paired kidney donation program would facilitate more transplants, reduce waitlist times, improve matching accuracy, and result in healthier and more satisfied patients. With enhanced public awareness and participation, we could have a positive impact on research, practice, and policy frameworks,” he added.
“In the end,” said Dr. Rees, “we hope these initiatives will lay the groundwork for changing the law in both countries so we can ultimately deliver more transplants.”
Open Question is a series of stories about innovative, solutions-focused research shaped to tackle pressing social problems.
